In the early days of the pandemic, one of the most talked about events – aside from the pandemic itself – was the toilet paper shortages.
Store shelves across the U.S. were empty for weeks as sales soared more than 700%. Folks were paying $10 or more just for one roll. People searched for toilet paper alternatives, like bidets.
It's something that we use every day, but most of us didn't think much about it before. But toilet paper hasn't been a regular part of life for long...
Prior to the mid-1800s, people used whatever was close by to clean themselves after using the toilet – like a sponge attached to a stick, a rag, an animal hide, a stone, a shell, a corncob, a square of paper from a magazine or a newspaper... (Except in China. According to ancient texts, the Chinese were using toilet paper in the sixth century, A.D.)
Then, in 1857, a New York inventor named Joseph Gayetty created a soft, perfumed, aloe-infused version of toilet paper. And having hemorrhoids became marketing fodder for the first U.S. toilet paper manufacturer, The Gayetty Firm.
Gayetty advertised this new paper as his medicated cure for hemorrhoids. He falsely claimed hemorrhoids were the result of wiping with paper containing "poisonous inks." Diet-induced constipation, however, was more likely to blame.
But while Gayetty's fearmongering wasn't enough to convince the masses that they needed this new product, other entrepreneurs – like the Scott Paper Company – soon followed in his footsteps and began making its own versions of toilet paper.
The thing is, most of us don't like talking about bowel habits, but hemorrhoids can be quite challenging. A few weeks ago, we received an e-mail from a reader that we couldn't ignore...
It was "signed, butt hurt (lol)." And while laughter is often considered the best medicine, it won't do much to heal your hemorrhoids. Our friend knows that hemorrhoids aren't just painful or itchy. They're also alarming when leaving bloody salutations on your toilet paper.
Hemorrhoids are common too, affecting one of every 20 people in the U.S., and around half of adults over age 50, according to the National Institute of Health.
But the actual numbers could be even higher, because lots of folks never bring this issue up with their doctor, opting instead to manage symptoms on their own. Some estimate that 75% of people in the U.S. will experience hemorrhoids at some point in their life.
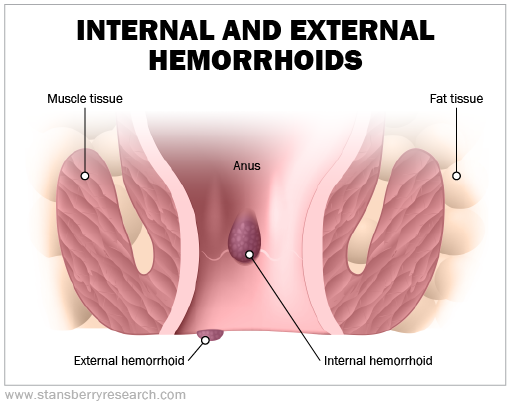
While some hemorrhoids are internal and some are external, the symptoms are generally the same. They include:
- Itching and irritation
- Pain or discomfort – although many internal hemorrhoids are painless
- Swelling or inflammation
- Bleeding while passing stool
- A hard lump near your anus if an external hemorrhoid forms a clot
Hemorrhoids develop when the veins around your anus stretch, bulge, and swell under pressure. This is more likely to occur as you get older. Pressure can arise from a number of scenarios, like:
- Straining during a bowel movement
- Sitting for long periods of time on the toilet
- Having chronic diarrhea or constipation
- Being obese
- Being pregnant
- Having anal intercourse
- Eating a low fiber diet, spicy foods, or drinking lots of alcohol
- Regular heavy lifting
Treating hemorrhoids varies depending on the location (internal or external) and severity of the problem. The severity of your hemorrhoid is graded by your doctor (grades one through four, followed by "complicated"), based on its appearance and size. Once the grade is established, medical treatment takes the following forms:
Grade 1 – Medication (like topical cream, systemic pill, suppository, or medicated wipes) or an office-based procedure (such as putting a rubber band around the base of the hemorrhoid, or injecting medication to make the vein shrink)
Grade 2 – Medication, office-based procedure, non-excisional operation (such as clamping-off or stapling the hemorrhoid), or excisional operation (hemorrhoid removal)
Grade 3 – Office-based procedure, non-excisional operation, or excisional operation
Grade 4 – Non-excisional operation or excisional operation
Complicated – Excisional operation
And lifestyle modifications are suggested at every level of severity. These modifications include keeping your stool soft through good nutrition and hydration, exercising regularly, avoiding sitting for long periods of time, and not straining on the toilet. Don't do what I do and sit and read on the toilet for long periods of time.
Often, increasing your fiber intake is recommended for hemorrhoid management.
The United States Department of Agriculture recommends eating 14 grams of fiber for every 1,000 calories of food you eat. So, for example, you need 28 grams of fiber if you eat 2,000 calories a day. Fresh fruit, vegetables, and whole grains are excellent sources of fiber.
But for folks with digestive issues – like irritable bowel syndrome, Crohn's disease, or ulcerative colitis – fiber can trigger a symptom flare.
Also, when adding fiber to your diet, do so gradually. And increase your water intake as you do this. Otherwise, you're likely to become constipated, and that will make your hemorrhoid even worse.
One last thing to note. Rectal bleeding can be a sign of colorectal cancer, so if you're concerned and your doctor brushes you off – like what happened to our friend "butt hurt" – tell them you'd still like an exam to rule out anything more serious.
So, whether or not you're able to use a little humor to make your hemorrhoids more bearable, there are a few different treatment options available to you. Eating well, hydrating, and moving your body every day are some of the best ways in which you can help yourself.
What We're Reading...
- Something different: After 35 years of recovery efforts, bald eagles are no longer considered endangered in Vermont.
Here's to our health, wealth, and a great retirement,
Dr. David Eifrig and the Health & Wealth Bulletin Research Team
March 8, 2022
