After a year in lockdown, we are finally starting to get some good news...
New COVID-19 cases and related hospitalizations are down. For many, it seems like light at the end of this year-long dark tunnel.
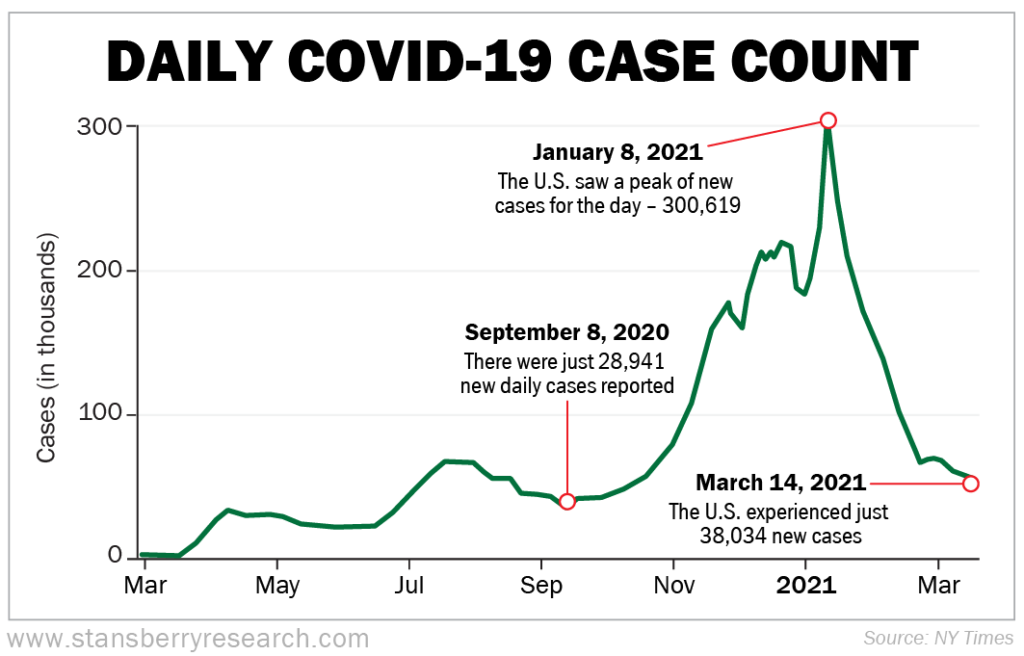
Take a look at COVID-19 case numbers...
On January 8, 2021, daily new cases in the U.S. peaked at 300,619. However, since then, they have been steadily decreasing, with a few upticks here and there.
On March 14, 2021, the U.S. had just 38,034 new cases. That's a low we haven't seen since September 8, 2020, when there were just 28,941 new daily cases reported.
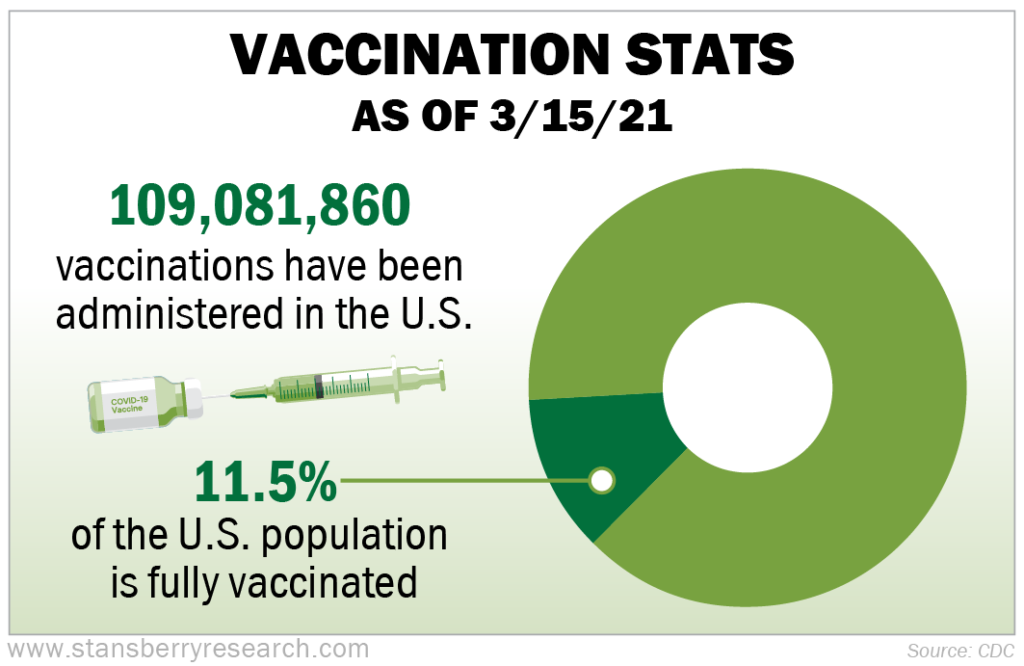
This change is likely the direct result of people finally reaching herd immunity as the end of year holiday gatherings led to the usual seasonal spreading of influenza-like illnesses... As of March 15, 2021, there have been 109,081,860 vaccinations administered in the U.S. So far, about 11.5% of the U.S. population is fully vaccinated.
Since the vaccine administration began, people have been posing with their vaccination cards and posting pictures on social media in both celebration and also to encourage others to do the same. This crowdsourcing technique has played an important role in building confidence in and support for the vaccine.
Let's take a closer look at where things currently stand with the COVID-19 virus and the various vaccinations available in the U.S...
THE VIRUS STRAINS
The COVID-19 virus is undergoing a type of transformation where different organisms independently evolve similar traits – known as convergent evolution. So far, there are six unique strains of the COVID-19 virus.
We see this convergent evolution in the similarities identified across the different strains of the virus: allowing the virus to evade the body's response to vaccines, for example – as seen in the New York and South African strains we'll detail in a moment.
Here are the strains we currently know about...
1. Wuhan – a.k.a. "Wildtype" – the original strain: This is the first strain that was identified in relation to this worldwide pandemic. It originated in the city of Wuhan, China in December of 2019 and rapidly spread across China and overseas. It reached the United States by early January 2020 after a man returned to the U.S. from Wuhan where he was visiting his family.
On January 30, 2020, the director general of the World Health Organization declared COVID-19 a Public Health Emergency of International Concern.
2. U.K. strain – a.k.a. B.1.1.7: This strain of COVID-19 became known in the fall of 2020. It's known to spread faster and more easily than the other variants and is considered more lethal than the Wuhan strain. It was first detected in the U.S. in December of 2020.
3. South African strain – a.k.a. B.1.351: This COVID-19 variation was originally detected in South Africa in October 2020, and it shares some of the same mutations as the U.K. strain. This strain seems the least responsive to the available vaccines and antibody therapies compared with the other strains. However, the treatments are still somewhat effective. This strain was first detected in the U.S. in January 2021.
4. Brazilian strain – a.k.a. P.1: This variant was first discovered in Japan in early January 2021, during the routine testing of people traveling from Brazil. It made its way to the U.S. by late January. The mutations in this strain make it more difficult for antibodies to recognize.
5. New York strain – a.k.a. B.1.526 (not yet peer reviewed): This strain was first detected in New York City last November and then popped up in isolated outbursts across the northeast. One of the mutations found in this form is similar to the South African strain in that it evades the body's response to vaccines.
This strain has yet to be peer reviewed, which is a routine part of scientific study. However, the research from both California Institute of Technology and Columbia University strongly support the existence of this strain.
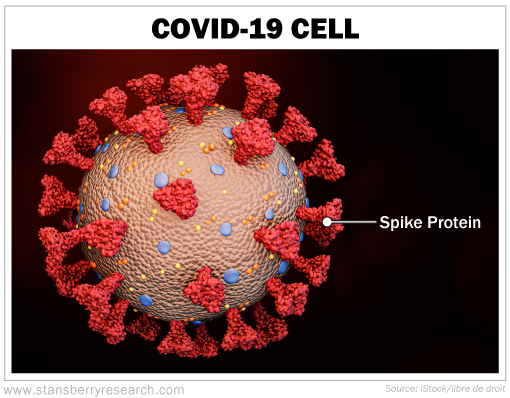
6. Californian strain – a.k.a. B.1.427/B.1.429 (not yet peer reviewed): This variant was first detected in California in September 2020. The mutation in this strain affects the spike proteins that protrude from the virus cell (shown in the photo below). This change is thought to allow this particular virus strain to attach itself more efficiently to other cells in the body, making it more infectious.
The research on this particular strain is also awaiting peer review, but studies have found it to be associated with more severe cases of infection and a higher risk of the need for oxygen intervention.
THE VACCINES
Vaccines train our bodies to make proteins – called antibodies – that fight disease without first making us sick, as would be the case if we were exposed to the disease itself. The science of vaccines – called vaccinology – has been around since 1796.
The three cells largely involved in our immune systems are macrophages, B-cells, and T-cells...
Macrophages digest cells and leave protein pieces behind – called antigens – that signal the body to send antibodies to destroy the antigens. B-cells produce the antibodies that destroy the antigens left behind by our macrophages. And T-cells attack the cells in the body that have already been infected.
Our cells display copies of this harmless spike protein piece on the surface of the harmful COVID-19 cells, and that signals which cells need to be destroyed. Once everything has been neutralized, our memory T-cells and B-cells have this experience to draw from for future infections.
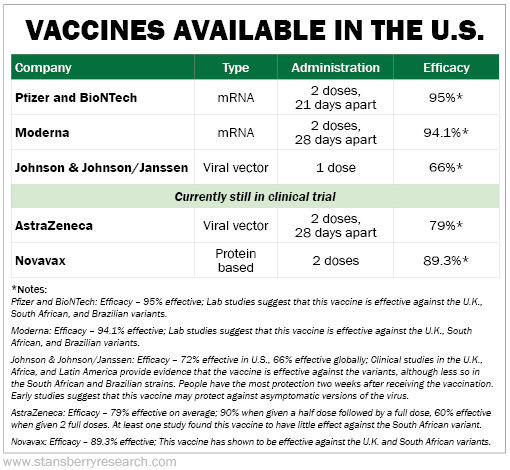
There are presently three different vaccines available and circulating in the U.S., and we have two vaccines still in testing phases. Of the five vaccines, there are three different mechanisms – or "types" – being utilized: messenger ribonucleic acid (mRNA), viral vector, and protein based.
The mRNA is a newly developed vaccine mechanism. It works by providing the cells in our immune system with the instructions needed to make a harmless piece of the spike protein that you would typically find on a COVID-19 cell.
Once made, the spike protein appears alien and it's attacked. It's then broken down by our immune system. Future white blood cells know just what to do because they have the memory encoded from the vaccine.
Viral vector vaccines are developed from several different viruses and also include a specific characteristic from the target virus – in this case, it's the COVID-19's spike protein. This combination of pieces of different viruses – like the adenovirus and SARS-CoV-2 virus – is what's known as the viral vector.
The viral vector then instructs the cells inside our bodies to create the spike protein and display it on the surface of harmful cells. This is the method by which this type of vaccine works, as opposed to the mRNA vaccine which delivers specific instructions for the cell.
You know what happens next... the "alien" proteins get neutralized as the antibodies and T-cells get to work.
Protein-based vaccines stimulate the immune system to respond to a disease that's being produced by an invading organism. It uses a harmless piece of the virus's spike protein (taken from an infected moth cell) and assembles the proteins into nanoparticles.
The nanoparticles mimic the molecular structure of the virus but cannot replicate or cause the virus itself. When these nanoparticles are injected into the body, they prime the body into producing antibodies and T-cells that would respond to a potential infection.
Unfortunately, we don't get to pick and choose which vaccine we get. When we show up for our shot, that's when we find out. Here's a general rundown on the vaccines we currently have:
WHO SHOULD GET VACCINATED?
Ideally, we want the first vaccinations to go to people who are vulnerable to complications from COVID-19 and those who are most likely to pass the virus onto vulnerable people. This means vaccines should be a priority for folks in states like Maine and Florida that have a high population of elderly people. And it should also be a priority for people who work in direct contact with others – like caregivers, people in the service industry, retail workers, health care workers, teachers, and certain government employees (mail carriers, sanitation workers, etc.).
That being said, I am choosing to forego the vaccine because I was directly exposed to the virus for several days in early December. Instead, I'm counting on my functioning immune system, which, last I checked, is still robust. But to be sure, I am getting my T-cell and B-cell immunity assessed to confirm whether I may need the vaccine or not.
Drop us a line and let us know what your plans are by e-mailing us at [email protected].
What We're Interneting...
- Go ahead, share your vaccine selfie.
- Check out the vaccine fact sheets for Pfizer, Moderna, and Johnson & Johnson/Janssen.
- Something different: Lightning bolts could have delivered the spark that started life on earth.
Here's to our health, wealth, and a great retirement,
Dr. David Eifrig and the Health & Wealth Bulletin Research Team
March 23, 2021