There is no silver bullet.
News came out this week that a group of doctors are now testing a heartburn drug, famotidine, as a treatment for COVID-19. It's just one of the latest drugs under investigation to treat this coronavirus disease.
But it isn't as promising as it sounds. The problem is that we just don't know what will work and why yet – we haven't focused on the mechanism of action. The mechanism of action is how something works – in this case, how the drug works in our body. We need to know what the drug interacts with, what changes it might cause, and any potential side effects there may be.
Worse, there's an urgency to find something that works and find it fast. But that leads to a lot of corner-cutting and potentially deadly oversight... not to mention untested off-label prescribing.
We've already seen a wealth of misinformation about other drugs like ibuprofen and angiotensin-converting enzyme ("ACE") inhibitors. Perhaps the most dangerous bit of misinformation: that hydroxychloroquine is our salvation. After all, what have you got to lose?
Turns out, you could lose your life.
This week, the U.S. Food and Drug Administration ("FDA") released a warning that we've worried about from the beginning: That two drugs touted as potential COVID-19 treatments, hydroxychloroquine and chloroquine (these two are related drugs), can trigger fatal heart problems.
What the news media skipped: Most of us already have a higher risk from taking these medications...
That's because hydroxychloroquine and chloroquine interact with many popular medications. And I'm not talking about mild reactions like sleepiness... I'm talking about significant changes in your heart's rhythm.
Drugs like these may have severe interactions when taken with hydroxychloroquine:
- Antianxiety (like Lexapro)
- Antiarrhythmic (like Pacerone)
- Antibiotics (like Cipro)
- Antidepressants (like Celexa)
- Antiemetics (anti-nausea) (like Anzemet)
- Antipsychotics (like Serentil)
Without getting too technical, some regular medications in these classes extend the intervals in heart rhythm a small amount. But combined with hydroxychloroquine, that interval can increase by a lot. Enough, in fact, to trigger deadly heartbeats (arrhythmias) or even sudden cardiac death.
And millions of folks take these medications. There were 270 million antibiotic prescriptions written for patients not in the hospital in 2015, according to Pew Research.
Plus, several other sources claim that about 13% of Americans are on antidepressants. That's more than 42 million Americans. With all the stress we're seeing from this crisis, we expect that number to jump up this year as well.
If you're taking any of these medications, you could be at a higher risk of serious heart problems should you take hydroxychloroquine.
In a recent issue of Nature Medicine, researchers from New York University School of Medicine shared early research on patients treated with hydroxychloroquine along with the antibiotic azithromycin.
They found more than 70% of folks had a change in their heart rhythm. And 11% of all patients had a change big enough that they were in danger of sudden cardiac arrest. Half of those with the dangerous change had normal heart measurements before the medication.
In other words, you're still at risk even if you aren't on any of these other medications. Which means if you are on them, your risk is even higher.
Now, chances are you won't need to be hospitalized for COVID-19 or use hydroxychloroquine, but that shouldn't stop you from preparing. News like this hammers home a point I've made many times: You need to be your own advocate.
So if you haven't already, you need to keep an updated list of all of your medications with you. Give a copy to every doctor you see and make sure your health care proxy has one – that's the person who can make decisions about your care should you be incapacitated.
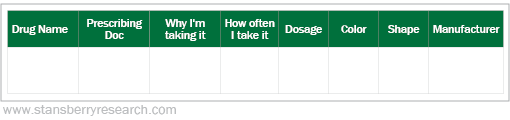
Here's what to include in your list: every medication you take, why you're taking it, the prescribing doctor, and the dosage. You'll also want to include all vitamins and supplements to make sure there are no interactions. And make sure to list any allergies you may have, especially any medications. Keep a journal like this:
These new findings shouldn't scare you, but it should make you more aware. Whatever you do, don't stop taking any prescription medication without consulting your doctor. Know which medications you take and make sure your doctors know the full list. It could save your life.
What We're Reading...
- More on the heartburn drug in the spotlight.
- Something different: The Navy confirmed UFOs?
Here's to our health, wealth, and a great retirement,
Dr. David Eifrig and the Health & Wealth Bulletin Research Team
April 30, 2020
